NUTRITION
Dietary fat intake – a complex issue
Limiting saturated fat continues to be a key healthy eating guideline for population health in Ireland
January 4, 2017
-
In recent times much confusion has arisen in the literature on optimal dietary fat intakes, particularly around the evidence for healthy eating advice to reduce saturated fat. The confusing findings emerging from long-term follow-up studies can be explained – but not simply.
Dietary guidelines for population health
On a global basis, dietary guidelines for human health in developed and developing countries are established by the World Health Organization (WHO). Different regions of the world adapt these global guidelines to suit their population needs. In Europe, the European Food Safety Authority (EFSA) adjusts the WHO guidelines into regional standards appropriate for the needs of people living in the EU. Similarly, the Institute of Medicine in North America develops the WHO guidelines into reference standards appropriate for the North American population.
In Ireland, national food-based dietary guidelines are developed to meet the specific needs of the Irish population and are based mainly on EFSA standards with Institute of Medicine (IOM) guidelines used where there are gaps.
Food-based dietary guidelines focus on protecting populations against nutrition-related diseases which contribute to mortality and morbidity.
In Ireland, the main contributors to ill health are cardiovascular disease (CVD) and cancer. Over the past three decades, the spiralling increases in obesity affecting all ages represents the most critical nutritional issue implicated in exacerbating several CVD risk factors (including type 2 diabetes) as well as directly increasing both CVD and cancer.
Overweight and obesity in Ireland are more evident in men and increase with age in both genders, indicating high-risk of metabolic syndrome, which is a clustering of risk factors that substantially increases CVD risk.
The metabolic syndrome is characterised by the presence of three out of five risk factors (abdominal distribution of body fat, elevated blood pressure, elevated fasting glucose, low HDL-C, high triglycerides).
Diet-lipid-heart disease hypothesis
Present-day knowledge on how dietary fat affects blood lipids has evolved over several decades. In the 1960s and 70s, after Dr Ancel Keys’ pioneering work linked dietary intake of saturated fat with blood cholesterol and CVD, blood lipid measurements mostly just involved total blood cholesterol.
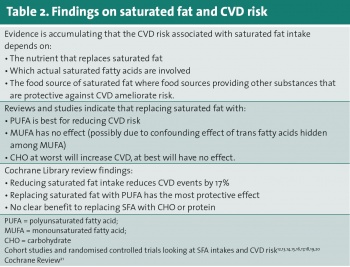
In these early days, dietary advice on fat was simple – saturated fat was identified as ‘the villain’ and PUFAn-6 as ‘the hero’. The benefits of other dietary fats (such as PUFAn-3 [eg. fish oils] and MUFA [eg. olive oil]) and detrimental effects of trans unsaturated fats were not appreciated until the 1980s/1990s, when blood lipid measurements included far more detail.
Then, in addition to learning about what dietary factors reduce harmful LDL blood cholesterol and maintain/raise the beneficial HDL fraction, knowledge on how diet affects other harmful blood lipid combinations (eg. low HDL and high triglycerides) revealed the importance of these other dietary fats, as well as many other dietary factors.
By the late 1980s, it was becoming clear that trans unsaturated fats were the real villains having much more detrimental effects on blood lipids compared with saturated fat. Trans unsaturated fat are mostly monounsaturated, but, for a time in Europe, hydrogenated marine oils were used, resulting in trans unsaturated fat including many polyunsaturated fatty acids also.
In general, dietary advice rarely distinguishes different fatty acids in the main classes of saturated, PUFAn-3, PUFAn-6 and MUFA. Distinguishing particular PUFAn-3 fatty acids from fish oil sources (eg. EPA and DHA) represent an exception.
Recently, claims that this is a significant oversight, especially in relation to saturated fat, have appeared in the literature. This view does not consider the distribution of the various saturated fatty acids in usual diets. The four saturated fatty acids that are most common in the Irish diet are all of longer chain length which, with one exception (stearic acid), have a blood cholesterol raising effect that extends to both LDL and HDL cholesterol fractions.
While stearic acid does not raise LDL cholesterol, it has been associated with increased tendency towards clotting (thrombogenesis), although the evidence is mixed. Other practical barriers to dietary advice at the individual fatty acid level include:
• The limitations of food composition tables regarding processed foods which constantly vary in fatty acid composition depending on fat source used (this is influenced by availability and cost)
• The impracticality of reflecting such complex and changeable information on food labels
• The legal requirements for nutrition labelling do not facilitate such additional information.
In summary, while it has been known for a long time that different saturated fatty acids have different effects on blood lipids, there is justification for dietary advice treating saturated fatty acids similarly, with the exception of stearic fat.
Stearic fat naturally occurs in cocoa and beef fat, so making some exception for dark chocolate (with a high cocoa content) may be warranted and this is always likely to be popular. However, due to the high energy density of dark chocolate, intakes need to be limited, even if the fat content is not particularly troublesome.
Based on strong evidence, the targets for optimal levels of blood lipids (LDL-C, HDL-C and triglycerides (TAGs)) have become much more stringent, especially for those at increased risk of CVD (presence of CVD, risk factors, diabetes etc). Healthy eating advice on fat focuses on achieving and maintaining optimal blood lipid levels in healthy and at-risk adults. However, the majority of those ‘at-risk’ require additional drug treatment (eg. statins) to achieve the very strict target blood lipid levels.
Throughout life, healthy eating advice on fat intake aims to slow down the gradual atherosclerotic process. From middle age, such advice includes a focus on prevention of thrombotic events (myocardial infarction or stroke) through inclusion of nutrients such as PUFAn-3.
Nutritional goals
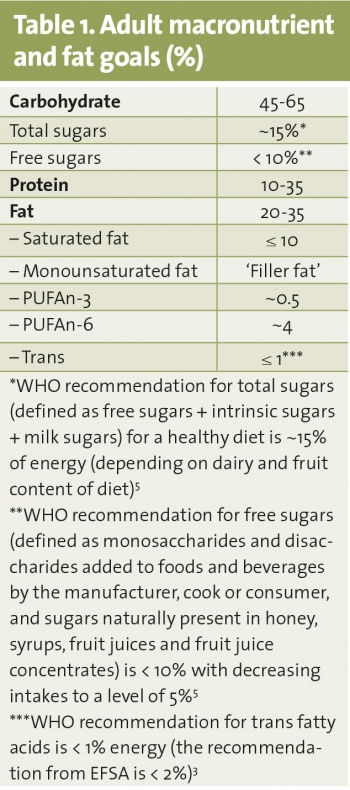
Diets providing a wide range of total fat can represent a healthy diet according to the recommendations of both EFSA and the IOM (20 – 35% energy).1,2 This flexibility allows for tailoring of dietary advice to suit varying needs at the individual level. Depending on genetic make-up and health status, some individuals (eg. those at increased risk of gastrointestinal diseases such as colon cancer) will benefit more from a low-fat, high fibre-rich carbohydrate intake (ie. > 50% energy), while others (eg. those at high risk of type 2 diabetes) do better on more moderate levels of fat intake and lower intakes of carbohydrate (ie. 40 – 45% energy). It should be noted that this flexibility does not extend to extreme reductions in carbohydrate (ie. 10 to 20% of energy) which, among other nutritional disadvantages, provide grossly inadequate intakes of fibre.
Notwithstanding variable overall levels of fat in the diet, there is global consensus that saturated fat intakes need to be kept ‘as low as possible’.2,3,4 Within this recommendation, it is recognised that some food sources of saturated fat are valuable sources of nutrients such as calcium and iron in the diet (eg. dairy and meat foods). Therefore, an upper limit of 10% of total energy intake is used for the development of food-based dietary guidelines that provide nutritionally adequate, low saturated fat diets.
Similar to overall fat intakes, there is corresponding flexibility inherent in the nutritional goals for overall carbohydrate intake levels because lower fat diets will be higher in carbohydrate and vice versa. However, just as there is consensus around the need to limit saturated fat, there is global consensus that added sugar in the diet needs to be limited as much as possible and that carbohydrates should primarily be complex and fibre rich in nature.
In most of the recent literature critically appraising healthy eating advice on fat and carbohydrate, there is awareness about the complexity of dietary fat, but not of dietary carbohydrate. Carbohydrate is made up of many different components and is equally, if not more, complex than dietary fat. In the simplest human health terms, some carbohydrates are beneficial (eg. components that are high in fibre and represent a complex mix of oligo-, and poly-saccharides) and some have adverse effects (refined carbohydrate low in fibre and high in sugar). The macronutrient goals for adults are outlined in Table 1 .
 (click to enlarge)
(click to enlarge)

 (click to enlarge)
(click to enlarge)