NUTRITION
RHEUMATOLOGY
Dietary impact on bone health
A balanced diet will optimise bone health by ensuring an adequate intake of calcium, protein and other micronutrients
July 1, 2012
-
Good nutrition is essential in building and maintaining strong bones. Osteoporosis, rickets and osteomalacia are diseases of the bone that have a major impact on health and quality of life across the lifespan in both developing and industrialised countries. Nutritional factors play important roles in determining the prevalence of these diseases.
Bone is a living tissue that is continuously undergoing a cycle of resorption and formation. The process of bone formation requires an adequate and constant supply of nutrients. Inadequate intake of nutrients important to bone increases the risk of bone loss and can have a major impact on the quality of new bone being formed.
Calcium and vitamin D play important roles in improving bone mineral density (BMD) and reducing the risk of fracture. Other nutrients that appear to also play a role in bone health include: protein, phosphorus, magnesium, zinc, vitamin C, vitamin K and fluoride.
Calcium
Calcium is perhaps the nutrient most commonly associated with bone health. It is estimated that 99% of calcium in the body is contained in the skeleton and teeth. Calcium’s main function is to provide rigidity and structure.1 Research highlights a beneficial relationship between calcium intake and bone health at various stages throughout the life cycle. 2-4
The new Irish food pyramid published only last month recommends three servings of dairy products a day for the majority of the population, which will provide approximately 800mg of calcium per day. Irish children and teenagers aged 9-18 years need five servings of dairy products a day (1,200mg).5 The previous recommendation for women in the second half of pregnancy or those lactating to have five portions of dairy products a day has now been reduced to in line with the general adult population of three servings of dairy products a day. Similarly the Institute of Medicine (IOM) recommends a calcium intake of 700-1,300mg/d for various life stage groups.
Milk and milk products are important sources of dietary calcium. They contribute 38% of the calcium intake in the diet of Irish adults aged 18-64 years.6 While the recent National Adult Survey reports that 16% of women aged 18-64 years had calcium intakes below recomendations,6 results from the Slán 2007 report highlight that some 61% of the Irish population eats less than the recommended minimum of three portions of milk/milk products a day.8
Milk and milk products contain calcium in large amounts and in a highly absorbable form. However, their fat content is often a cause for concern, particularly as cardiovascular disease and obesity are growing issues in the Irish population. Reassuringly, milk and milk products are available with varying fat content and low fat versions of dairy products have similar calcium, protein and B-vitamin levels to full fat versions.9 Although calcium is also available in a wide variety of non-dairy foods, the amount of calcium that can be absorbed from these foods, the amount of calcium per portion and the frequency with which they are consumed often makes them unreliable sources to optimise bone health.
Certain components of plant foods can affect calcium absorption. These include phytates and oxalates, which are found in foods such as nuts, grains, spinach, rhubarb and beans. Phytates and oxalates cause insoluble complexes with calcium, reducing absorbability. To highlight how this impacts on the calcium content of our diet we can compare a serving of milk to a serving of spinach: to obtain the same amount of calcium as from a glass of milk, you would need to eat 16 portions of spinach.10 Approximately 30% of calcium from milk is absorbed, compared to only 5% in spinach.11,12 Soy is a notable exception – despite the presence of oxalates and phytates, the calcium in soy is highly absorbable and comparable to milk. However, the calcium content of soy milk is only one sixth the calcium content of cow’s milk.10 In practical terms this would suggest that people avoiding dairy products should choose a calcium fortified soy milk as an alternative to cow’s milk.
There are many plant foods with a low oxalate content that provide calcium in an highly absorbable form. These include vegetables such as broccoli, bok choy and kale.10,13 However, the overall calcium content of these foods is low, making them an unreliable source of calcium in the daily diet. Other sources of calcium in the diet include oily fish with soft edible bones such as sardines and anchovies, but again, the frequency with which foods are eaten do not make them a reliable source of calcium.14
Ultimately, milk and milk products are the most reliable and absorbable form of calcium in the diet. Other foods high in calcium should be considered as a way to boost calcium intake in a dairy rich diet. Where milk and milk products are not eaten with sufficient frequency, calcium supplements and calcium fortified foods provide a way to enhance the calcium content of the diet.
Vitamin D
Vitamin D is a fat-soluble vitamin that is found in certain foods. It is also produced on our skin when it is exposed to sunlight. Vitamin D is required for calcium absorption and plays a key role in calcium homeostasis – mainly by regulating calcium absorption and excretion. It also has a direct effect on bone, stimulating bone formation and resorption. Severe vitamin D deficiency causes poor quality bone to be formed leading to osteomalacia in adults and rickets in children. Low vitamin D levels are also associated with lower bone mineral density.15 Vitamin D production is affected by season, latitude, duration of exposure to sunlight, sunscreen use, skin pigmentation and the ability of the skin to form and process vitamin D. Vitamin D inadequacy is widespread worldwide. Studies in Ireland have revealed that low vitamin D status and vitamin D deficiency are widespread in the Irish population.16
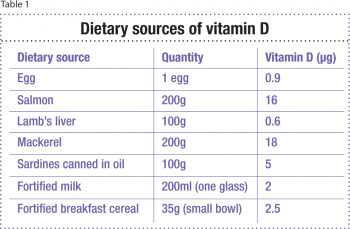
Dietary sources of vitamin D include oily fish, fish oils, eggs and foods fortified with vitamin D. The National Adult Nutrition Survey in 2011 revealed that the main sources of vitamin D in the Irish diet were meat, fish and spreads.6 Irish people are often reliant on dietary intake of vitamin D to satisfy their requirements due to our northerly latitude. However, foods naturally rich in vitamin D are few in number and in many cases not widely consumed. Table provides examples of dietary sources of vitamin D.
 (click to enlarge)
(click to enlarge)
