MENTAL HEALTH
Prescribing pressures – a heavy burden for GPs
While GPs are being urged to reduce prescriptions for benzodiazepines and z-drugs, there is immense pressure from patients who have become dependent
October 1, 2013
-
Benzodiazepines, and more recently z-drugs as hypnotics, are some of the most widely prescribed medications in general practice. Most literature highlights their safety in short-term prescribing and their effectiveness for anxiety and insomnia, but warns that dependence is a significant risk which can set in after one month.1
The withdrawal of benzodiazepines can replicate the original symptoms for which they were prescribed. GPs frequently report pressure from patients to prescribe benzodiazepines for their anxiety and also resistance from patients when attempts are made to reduce current dosages.
The Department of Health has produced guidelines on benzodiazepine prescribing, which again highlight the importance of only prescribing these drugs for short periods in order to avoid addiction or dependence. For new patients, GPs are advised to initiate the lowest dose which needs to be adjusted depending on response and also that the prescription should be for not longer than four weeks. The risks of dependence need to be discussed and the advice recorded in the patient’s file.2
For dependent patients on long-term benzodiazepines, the GP is advised to issue small quantities at a time with regular review. Again it is advisable to make patients aware of the long-term risks and that this is documented.
Qualitative research has shown that GPs are likely to maintain the patient on a benzodiazepine prescription if another GP has commenced prescribing benzodiazepines. In Australia, many GPs remain reluctant to initiate dose reduction in older patients or if the patient has been on them for a long time.3 Adding cognitive behavioural interventions is said to be helpful to GPs in their efforts to achieve cessation of benzodiazepine use. However, it is noticeable that in such studies recruitment of patients has been difficult, with the more motivated more likely to be enrolled in such studies.4
The HSE has recently provided GPs with reports on benzodiazepines and z-drug prescriptions for November 2012. It allows GPs to compare benzodiazepine prescribing with that of peers.
Audit
In a practice in a deprived urban area we decided to audit long-term benzodiazepine prescribing, which was defined as the regular collection of a prescription for benzodiazepines or z-drugs over the previous six months. A plan was devised where all such patients were required to see the GP for their next prescription when their benzodiazepine and z-drug consumption was discussed with a view to reduction or cessation, if appropriate. Patients were provided with a practice leaflet highlighting the purposes and side-effects of benzodiazepines and z-drugs. The leaflet also described the effects of withdrawal and the support available in the practice and is available from the authors. The practice has a Level 1 methadone prescribing contract.
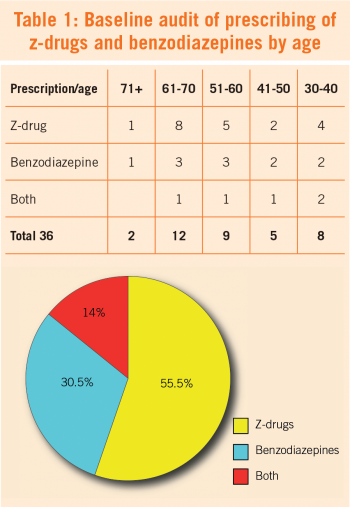
Some 36 patients out of a GMS list of 917 were identified as regular long-term benzodiazepine and z-drug users. Of these, 32 were female and the practice profile is of young and middle-aged patients: eight were in the 30-40 age group, five in the 41-50 age group, nine aged from 51-60, 12 in 61-70 age group and two were over 71. A breakdown of the 36 prescriptions showed that 20 patients were prescribed z-drugs, 11 were prescribed benzodiazepines and five patients were receiving both benzodiazepines and z-drugs (see Table 1).
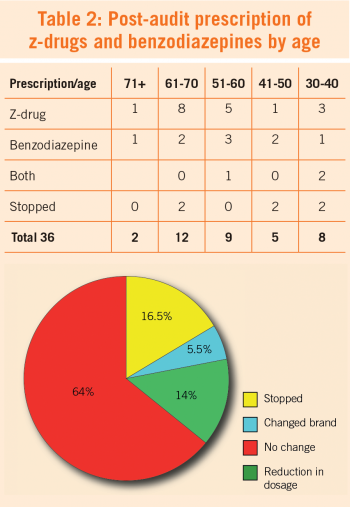
On review of the 36 patients at three months, six had stopped taking benzodiazepines, two changed from one brand to another and five had reduced their benzodiazepine dosage. This left 23 patients (64%) in whom it was not possible to effect any change or reduction in prescribing. One of the patients who stopped receiving prescriptions was later identified as buying on the street (see Table 2).
Discussion
The HSE report identified the practice as slightly below the national prescribing average but it under-reported the number of patients on benzodiazepines. Considerable effort was required from the practice in negotiating with this group of patients and in advising them on the negative effects of benzodiazepines. While our efforts had some success it evoked resistance from many patients and caused fear and anxiety in a small number. Many patients have been receiving benzodiazepines for much longer than six months, with some being started before they moved to the practice. Street availability is a factor in any intervention in benzodiazepine use as it was in the audit.
The majority of patients on benzodiazepines and/or z-drugs were female. The practice may view males requesting benzodiazepines in a different light than females. Most of those on the practice methadone programme are males and there is more caution about introducing another addictive substance, particularly for young men. The size of the sex difference is however striking and worthy of more investigation.
While the literature exhorts GPs to prescribe with due care, GPs have not articulated the pressure they are under to prescribe benzodiazepines even for short-term use and particularly to maintain patients who are on longer term prescriptions. This audit reports modest success after three months and as experience shows this success is likely to be watered down over time.
Acknowledgements
Special thanks to Lily Kilbride for engaging the patients in the audit and to Dr Brendan O’Shea for encouragement to write it up.
 (click to enlarge)
(click to enlarge)

 (click to enlarge)
(click to enlarge)