CARDIOLOGY AND VASCULAR
ENDOCRINOLOGY
Prevalence of thyroid disease in patients with atrial fibrillation
A study by the cardiology team at St Luke’s Hospital, Kilkenny, found thyroid function assessment to be beneficial for all patients with atrial fibrillation to avoid complications
October 1, 2014
-
Atrial fibrillation (AF) is the most common arrhythmia in clinical practice and accounts for at least a third of hospitalisations due to cardiac rhythm disturbance.1 Paroxysmal and persistent AF affects 2.2 million Americans and six million Europeans.1,2 Patients with AF also have increased risk of impaired cognition,3 quality of life and exercise capacity, left ventricular dysfunction, and five-fold increase risk of stroke, resulting in increased health provision cost.4,5
Thyroid dysfunction is one of the disabling treatable risk factors for AF.6,7 Recent data have shown that overt hyperthyroidism and subclinical hyperthyroidism, which has the prevalence of 10-25% in elderly patients,7,8 have been associated with significant increased risk of AF.8 Current guidelines advise aggressive treatment for patients with subclinical hyperthyroidism,9 so as to avoid other complications (for example, impaired ventricular relaxation, reduced exercise tolerance and increased risk of atherosclerosis, hence infarction and cardiovascular mortality) associated with subclinical thyroid disease.10,11
Aim
This study aimed to assess the prevalence of thyroid disease in patients presenting with AF in our area. It also aimed to assess the management of their abnormal thyroid status.
Methods
Conservative presentations of patients to hospital with known or new paroxysmal, persistent and permanent AF over a period of 12 months were recorded. Initial data was retrieved from the Hospital Inpatient Enquiry (HIPE) system. Further data was collected from patients’ clinical notes, the laboratory database and from general practitioners. Data collected included age, sex, thyroid function status and co-morbidities.
Thyroid status was assessed by the level of thyroid stimulating hormone (TSH). Euthyroidism was defined by thyrotropin levels from 0.27 to 4.2mIU/L and subclinical hyperthyroidism when thyrotropin was less than 0.27 but normal free thyroxine levels when patients were not on thyroid-altering medications.
Results
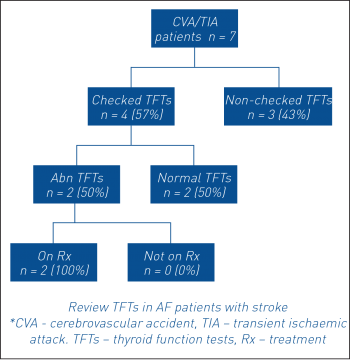
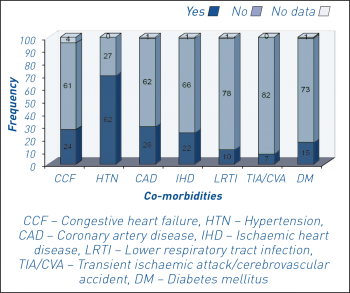
A total of 501 presentations, including 110 patients, were recorded over a period of 12 months. Mean age was 72 ±11 years (range 41-94 years). Some 21 patients were excluded as their clinical notes could not be found. Of the remaining 89 patients, there were 49 males and 40 females. Mean length of stay was three days (R 1-16 days). Thyroid function status was assessed in 87% (n = 77) of AF patients with mean TSH of 3.08mIU/L (R 0.22 to 30.5mIU/L) (see Figure 1).
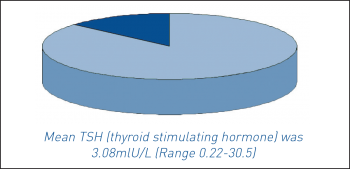 Figure 1. Assessment of thyroid function tests in patients with atrial fibrillation in St Luke’s Hospital(click to enlarge)
Figure 1. Assessment of thyroid function tests in patients with atrial fibrillation in St Luke’s Hospital(click to enlarge)

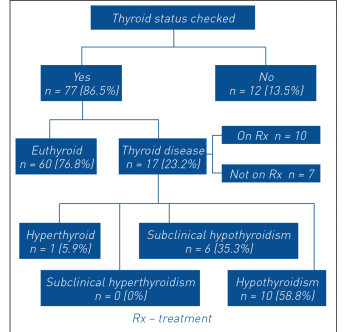 Figure 2. Thyroid function assessment and intervention(click to enlarge)
Figure 2. Thyroid function assessment and intervention(click to enlarge)