MENTAL HEALTH
Psychosis and schizophrenia: importance of early referral
Better understanding of the natural course of schizophrenia will help early detection
February 9, 2015
-
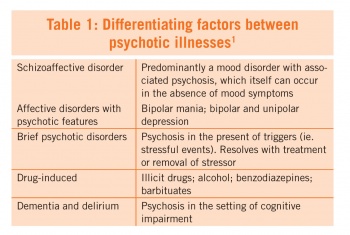
Psychosis is a ‘disturbance in the perception of reality, evidenced by hallucinations, delusions, or thought disorganization’.1 It affects 4-5% of the population and occurs in a variety of psychiatric illnesses (see Table 1).1,2 It is characterised by hallucinations (auditory hallucinations are the most common subtype), delusions (ie. false fixed beliefs), thought disorganisation, agitation and aggression.2
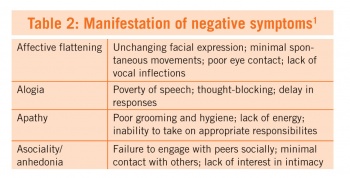
Schizophrenia affects 1% of the population. It is a chronic psychiatric illness with periods of active psychosis combined with a decline in day-to-day function.4 Symptoms are divided into: positive, negative, cognitive and affective. Positive symptoms are synonymous with active psychosis (ie. hallucinations, delusions and disorganised behaviour and thinking); where auditory hallucinations occur in 40-80% of patients.4 Negative symptoms consist of affective flattening, alogia, apathy and asociality/anhedonia (see Table 2). These moderately correlate with functional impairment and tend to be resistant to treatment.3
Cognitive symptoms correlate with loss of function and usually precede the onset of positive symptoms.1,4 Areas that are affected include processing speed, attention, visual learning and memory, executive function, verbal comprehension and social cognition. Lastly, affective symptoms (mainly depression) occur in over half of patients throughout the course of their illness.
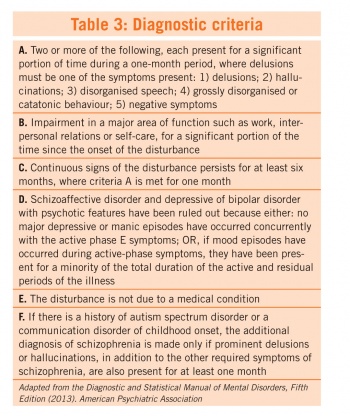
The American Psychiatry Association updated the diagnostic criteria for schizophrenia in 2013 and Table 3 summarises these criteria.
Schizophrenia is one of the most debilitating and economically catastrophic medical disorders.4,5 Life expectancy is reduced by 10 years and only 10% will make a recovery allowing them to function completely independently within society.5 The duration of untreated psychosis correlates to poorer outcomes and it is associated with resistance to treatment, increased relapse rates, faster cognitive decline, increased risk of depression and substance abuse and increased incidence of behavioural problems.5 As such, early referral is crucial and re-enforces GPs’ pivotal role in early recognition of the disease.5,6
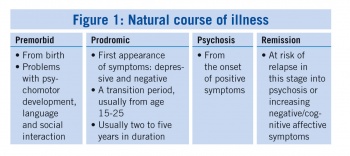
Delayed diagnosis occurs more frequently in men, with earlier age of onset, and in those with a prolonged prodromal phase and fewer early positive symptoms.6 Studies have shown that 68% of patients present insidiously and attend their GP five to six times in the prodromal phase prior to accurate diagnosis.5 Better understanding of the natural course of this illness may help early detection (see Figure 1).
Early detection is understandably difficult as the symptoms at this stage are usually non-specific.5 Patients may present, or usually are brought in by a relative prior to the development of positive symptoms. A decline in hygiene or grooming and a reduction in psychomotor activation may precede the active psychotic phase.4 Such changes are important to note and can aid early diagnosis. Negative, cognitive and affective symptoms occur earlier in the course of the illness, so one should always think of screening for psychotic symptoms in anyone presenting with these types of symptoms.
It is important to take into account risk factors for developing psychosis such as family history of schizophrenia, history of intermittent psychotic symptoms, social isolation, and history of intra-uterine or perinatal complications.5,7
When a patient presents with features suggestive of psychosis, it is essential to fully investigate any possible underlying causes, as per common medical work-up:
- Bloods: FBC, U+E, LFT, TFT, B12, Ca, folate, VDRL (if indicated), urine C+S, toxicology screen, HIV (if suspected)
- Other investigations to consider: CT brain or MRI, EEG, lumbar puncture (if indicated), heavy metal screen, rheumatologic work-up, hormone levels.8
Any underlying causes should be treated. Use of antipsychotic should be commenced where relevant and in some instances benzodiazepines may be used for symptom management in consultation with psychiatric services.
Agitated patients should be evaluated for risk of harm to themselves or others and one should consider whether an involuntary admission under the Mental Health Act 2011 is appropriate. A rapid-acting first generation antipsychotic (eg. haloperidol) and/or a rapid-acting benzodiazepine (eg. lorazepam) should be used in severely agitated patients with acute psychosis.
Treatment of schizophrenia should take into account biological, psychological and social factors involved with the disease. Antipsychotic drugs, when taken regularly, protect against relapse in the short- and long-term.
 (click to enlarge)
(click to enlarge)

 (click to enlarge)
(click to enlarge)
 (click to enlarge)
(click to enlarge)
 (click to enlarge)
(click to enlarge)