RHEUMATOLOGY
CANCER
PAIN
WOMEN’S HEALTH
SURGERY
Sacroiliac joint dysfunction – a common cause of low back pain
The most common cause of sacroiliac joint pain is idiopathic and may occur acutely or insidiously with cumulative trauma
May 1, 2015
-
The sacroiliac joint (SIJ) is the largest axial joint in the musculoskeletal system and its primary responsibility is to transfer the weight of the upper body to the lower extremities. In the past this joint has been largely ignored as a pain generator, however, recent research has reported that the sacroiliac complex may be the source of pain in 15-25% of all individuals who present with low back problems.1 To avoid unnecessary lumbar spine surgery, SIJ disorders should be strongly considered in low back pain diagnosis.2
Anatomy
The sacroiliac joints are composed of the sacrum wedged between the ilia. It is the largest axial joint in the human body, with a surface area of approximately 17.5cm2. The morphology of the SIJ not only changes with age but it also varies greatly in size, shape and contour from side to side as well as between individuals.
The surface of the joint is flat until after puberty. By age 30, bony ridges are present on the articular surface of the ilium. With time the synovial articular surfaces erode and the synovial cleft narrows. The joint is supported by numerous ligaments, muscle and fascia.
Biomechanics
The SIJ functions as a shock absorber, forms a base for the spinal axis, transmits and dissipates upper trunk loads, and facilitates childbirth. Motion in the SIJ is limited to small amounts of rotation and translation.
Compression of the sacrum with weight bearing creates a ‘keystone in an arch’ effect: the greater the force through the sacrum, the greater the resistance.
Pathology
The most common cause of SIJ pain is idiopathic and may occur acutely or insidiously with cumulative trauma. Idiopathic SIJ pain may result from a change in the joint’s position or mechanics. Other potential causes include:
- Trauma
- Osteoarthritis
- Infection
- Inflammatory conditions (sacroiliitis is present in virtually 100% of individuals with ankylosing spondylitis)
- Metabolic conditions (for example, gout and renal osteodystrophy)
- Malignancy – metastases to the pelvis account for 40% of all osseous metastasis, second only to those of the spine and iatrogenic, for example, post bone graft harvesting, lumbar spine fusion).
Insufficiency sacral fractures in the older osteoporotic patient may occur with little or no trauma, and can be difficult to visualise on plain radiographs. Stress fractures have been reported in athletes due to repetitive microtrauma caused by impact loading over long periods of frequent physical exertion.
The third trimester of pregnancy results in hypermobility of the sacroiliac joint because of increased levels of oestrogen and relaxin that cause the soft tissues supporting the joint to loosen. This laxity may predispose the sacroiliac joint ligaments to painful sprain. The mechanical trauma of childbirth also may cause joint pain.
Diagnosis
History: Patients with pain originating from the SIJ may complain of a number of different symptoms including:
- Low back pain
- Lower extremity pain (numbness, tingling, weakness – usually above the knee)
- Buttock pain
- Hip or groin pain.
Functional symptoms, which may be more specific in identifying the SIJ as the source of pain, include:
- Unilateral leg instability (buckling, giving way)
- Disturbed sleep patterns
- Disturbed sitting patterns (unable to sit for long periods on one side, such as when driving)
- Transitional symptoms (pain going from sitting to standing or supine to standing)
- Pain on the affected side with stair use.
Examination
The clinical examination begins with excluding the lumbar spine and hip joint as the main sources of pain with negative screening exams. The following are then performed to isolate the SIJ as the primary source of pain:
Fortin test – while standing, have the patient point with one finger to the location of pain, this test is positive if the patient points on two occasions to the area directly medial and inferior to the posterior superior iliac spine (PSIS) (Figure 1)
 Figure 1. Fortin’s finger test(click to enlarge)
Figure 1. Fortin’s finger test(click to enlarge)

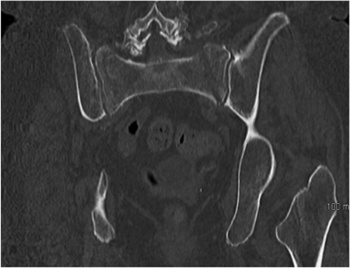 Figure 2a. Coronal pelvic CT of 68-year-old female with chronic ‘low back pain’ demonstrating bilateral sacral insufficiency fractures(click to enlarge)
Figure 2a. Coronal pelvic CT of 68-year-old female with chronic ‘low back pain’ demonstrating bilateral sacral insufficiency fractures(click to enlarge)
 Figure 2b. Plain film pelvic x-ray six months post percutaneous fixation of bilateral sacral insufficiency fractures(click to enlarge)
Figure 2b. Plain film pelvic x-ray six months post percutaneous fixation of bilateral sacral insufficiency fractures(click to enlarge)