HEALTH SERVICES
Successful rapid improvement event to improve patient flow
A report on a rapid improvement event in one AMAU which aimed to increase patient flow through the department and improve patient experience time in accordance with the National Acute Medicine Programme
June 28, 2019
-
Acute medical assessment units (AMAU) improve the efficiency in the admission process for unplanned patients by providing assessment, investigation and management of acute medical patients. The emergency department stay is eliminated or drastically reduced in this model of care. AMAU provide specialist physician assessment, review and evaluation of the patient at point of entry to hospital.
The AMAU at Wexford General Hospital conducted a rapid improvement event in June 2018 to improve patient flow through the department and improve patient experience time (PET) in accordance with the National Acute Medicine Programme (NAMP).
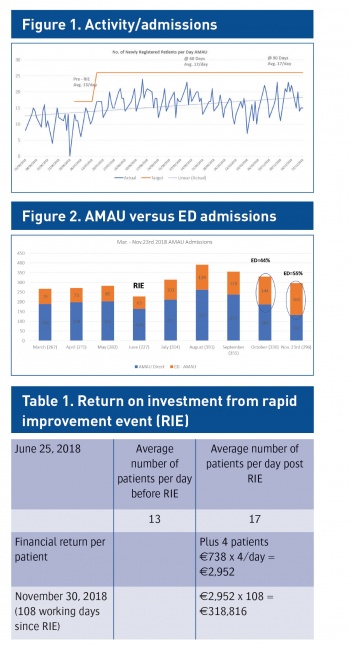
In supporting the Ireland East Hospital Group (IEHG) unscheduled care programme, a key priority is the need to increase the flow of patients through and have a fully operational AMAU. In June 2018 the AMAU was open Monday to Friday 8am-9pm, with last patient admission by approximately 3pm. There were approximately 13 patients per day flowing through AMAU and the potential demand was found to be greater than available capacity.
Aims of the project
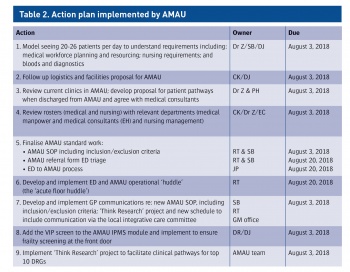
The aim was to improve the flow into and increase the flow of patients through AMAU. Specifically to:
- Identify staffing requirements for the 5/7 service operating 12-14 hours per day
- Determine the appropriate medical patient pathways to AMAU:
– GP direct to AMAU
– Direct admission to relocation of patients from ED to AMAU transfer, admission or discharge and related logistics
– Stream patients from out-of-hours CareDoc/GP from ED to AMAU where possible
- Meet critical AMP quality and safety indicators:
– First seen by a nurse (20 minutes)
– First seen by a doctor (60 minutes)
– Six-hour patient experience time (discharge or admit)
– Admit/discharge rates.
 (click to enlarge)
(click to enlarge)

 (click to enlarge)
(click to enlarge)