CARDIOLOGY AND VASCULAR
Thromboembolic prophylaxis
Following an audit of the use of thromboprophylaxis in non-surgical inpatients, a team of doctors recommend the incorporation of a risk assessment model into medication records
August 1, 2015
-
Venous thromboembolism encompasses two inter-related conditions that are part of the same spectrum, deep venous thrombosis (DVT) and pulmonary embolism (PE). DVT and PE are associated with significant mortality and morbidity.1 Hospitalised patients are 100 times more likely to have VTE,2 compared to patients in the community. Around 5-10% of all-cause in-hospital mortality is due to PE.1,3 Postmortem studies have revealed that nearly 70% of fatal PEs occurs in non-surgical patients.1
Thromboembolic disease is the third most common acute cardiovascular disease, after cardiac ischaemic syndromes and stroke.4 The spectrum of disease ranges from asymptomatic to massive embolism causing death, and indeed DVT and PE frequently remain undiagnosed because they may not be suspected clinically. Untreated acute proximal DVT causes clinical PE in 33-50% of patients. Untreated PE is often recurrent over days to weeks and can either improve spontaneously or cause death. VTE prophylaxis is important and all hospitalised medical patients should be assessed for VTE risk and prescribed medications accordingly.
Objective
We set out to conduct an audit on prescribing appropriate thrombo-prophylaxis for hospitalised non-surgical patients in a regional hospital.
Materials and method
This was a prospective data analysis. The patients were adults (over the age of 18 years) of both gender admitted under the medical team from March 14, 2015 to March 20, 2015. Inpatient charts during this period were reviewed and data was recorded in a predesigned structured proforma. Exclusion criteria included: age less than 18 years, non-inpatients (outpatients department, medical assessment unit, emergency department attendees) and patients admitted to hospital with a diagnosis of DVT or PE.
Results
The total number of inpatient charts reviewed during this period was 158. Of these, 50 patients were selected and divided into three age groups:
- The first group for patients <50 years of age, which comprised 6% (3) of patients
- The second group for those 50-70 years of age, which comprised 32% (16) patients
- The third age group for those in the elderly age group (> 70 years), which comprised 62% (31) of patients.
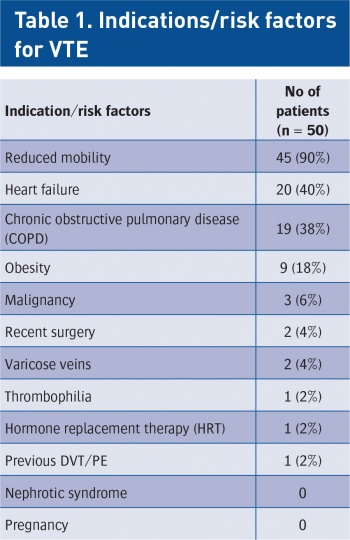
There were slightly more males (54%; 27) than females (46%; 23) in the study. The most common risk factor for thromboembolic phenomenon was found to be reduced mobility for more than three days, which was present in 90% (45) of patients. Risk factors are shown in Table 1. Most of the patients had more than two risk factors including: heart failure (present in 40% [20] of patients), chronic obstructive pulmonary disease (present in 38% (19) of patients), obesity in 18% (9) and malignancy in 8% (4) of patients. Other risk factors were recent surgery and varicose veins in 4% (2); thrombophilia and patients on hormone replacement therapy were found in only 2% (1) of patients.
The total number of patients who received prophylaxis was 54% (27) and the number of patients who did not receive prophylaxis was 46% (23). This could be due to a reason not charted by the team or due to contraindications. The most common treatment given in these patients was enoxaparin, which was given in 20% (10) of patients, while 14% (7) of patients were on oral anticoagulant/antiplatelet therapy, 14% (7) of patients were on low molecular weight heparin (LMWH) plus an oral anticoagulant, and 2% (1 each) were on just compression stockings, enoxaparin plus compression stockings, and tinzaparin respectively.
 (click to enlarge)
(click to enlarge)

 (click to enlarge)
(click to enlarge)