RESPIRATORY
A case of bilateral pulmonary artery hypertrophy
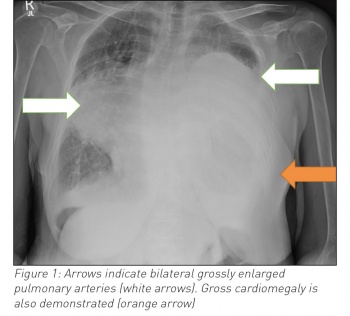
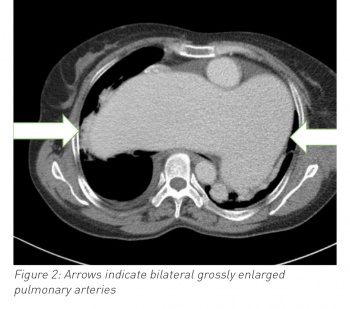
A case of respiratory failure caused by pulmonary artery hypertension with severe hypertrophy on chest x-ray
October 2, 2017
-
Pulmonary hypertension is an uncommon disorder characterised by mean pulmonary artery pressure ≥25mmHg. It has multiple aetiologies and has a prevalence of 5-50 per one million people.1 In this case we report on a case of respiratory failure caused by pulmonary artery hypertension with severe hypertrophy on chest x-ray.
Case
A 54-year old woman with a history of pulmonary stenosis, pulmonary hypertension (of mixed aetiology), mitral regurgitation and atrial fibrillation presented to the emergency department with chest discomfort and worsening dyspnoea. She was tachycardic, tachypnoeic (at 48 resp/min) with oxygen saturations of 72% on 4L O2. Cardiovascular and respiratory system examination revealed a loud pan-systolic murmur, diffuse wheeze and pitting oedema to the mid-thigh.
Blood work showed a neutrophilia, hypochromic anaemia, elevated C-reactive protein and an acidotic type two respiratory failure. A chest radiograph was significant for an opacity in the lower two-thirds of the left lung field and a second opacity in the right mid-zone. Given the woman’s past history the differential included right-sided pneumonia, left-sided pleural effusion and cardiomegaly, or hypertrophied pulmonary arteries.
A computed tomography scan confirmed grossly hypertrophied pulmonary vasculature.
Despite intubation, ionotropic and anti-microbial support this woman passed away in the intensive care unit after five days.
 (click to enlarge)
(click to enlarge)

 (click to enlarge)
(click to enlarge)