MENTAL HEALTH
An introduction to DSM-5
The long-awaited fifth edition of the Diagnostic and Statistical Manual of Mental Disorders has arrived: what's new?
September 1, 2013
-
In this short article the author attempts a skeletal summary of the Diagnostic and Statistical Manual of Mental Disorders, fifth edition (DSM-5), published by the American Psychiatric Association (APA) in 2013.
DSM-5 classification
Neurodevelopmental disorders
Neurodevelopmental disorders are of early onset, often before starting pre-school. Developmental deficits cause impairments of personal, social, academic or occupational function. Many patients formerly labelled with Asperger syndrome would now be diagnosed as having autism spectrum disorders “without language or intellectual impairment’’. Intellectual disability (‘‘intellectual developmental disorder’’ in ICD-11) can be mild, moderate or severe; “global developmental delay” is used when the patient is less than five years old and clinical severity cannot be assessed. “Unspecified intellectual disability” is used for people over five years of age and clinical severity cannot be assessed. Communication disorders are language problems (such as poor word knowledge or use, poor sentence construction, difficulty explaining and conversing), speech sound difficulties (interfere with intelligibility and prevent good verbal communication), stuttering (childhood-onset fluency disorder) and social (pragmatic) communication. Autism spectrum disorders involve deficits in social-emotional reciprocity, non-verbal communication, and developing, maintaining and understanding relationships; stereotyped/repetitive motor movements or use of objects or speech, insistence on sameness, highly restricted or fixed interests (abnormal in intensity and focus) and excessive over- and under-reactions to sensory input or unusual interest in sensory aspects of the environment. Attention-deficit/hyperactivity disorder (ADHD) and specific learning disorder (reading, writing, maths) appear basically unchanged. Motor disorders include developmental co-ordination disorder (clumsy child syndrome), stereotypic movement disorder (+/- self-injury) and tic disorders (Tourette, persistent/chronic motor or vocal).
Bipolar and related disorders
Bipolar (BP) and related conditions include BP I disorder, BP II disorder (hypomania is less impairing than mania and does not lead to hospitalisation), cyclothymic disorder, substance/medication-induced BP disorder and cases due to another medical disorder. Depressive disorders include disruptive mood dysregulation disorder, major depressive disorder (with/without psychotic features; single episode/recurrent; specify if with anxious distress, mixed features, melancholic features, atypical features, mood-congruent or mood-incongruent psychotic features, catatonia, peripartum onset, or seasonal pattern, the last applying only to recurrent episode), persistent depressive disorder (dysthymia), premenstrual dysphoric disorder, substance/medication-induced depressive disorder and depressive disorder due to another medical disorder.
Anxiety disorders
Include separation anxiety disorder, selective mutism, specific phobia (animal, blood-injection/other medical care, situational and “other”), panic disorder, panic attack, agoraphobia, generalised anxiety disorder, substance/medication-induced anxiety disorder, and anxiety disorder due to another medical condition.
OCD and related disorders
Obsessive-compulsive disorder (OCD) and related disorders include OCD itself, body dysmorphic disorder (with/without muscle dysmorphia), hoarding disorder (with/without excessive acquisition of items that are not needed or cannot be stored – state level of insight and presence/absence of delusions), trichotillomania (hair-pulling disorder), excoriation (skin-picking) disorder (leads to skin lesions and patient tries to stop the behaviour), OCD and related disorders due to substance/medication or another medical condition. An “other specified” group includes body dysmorphic-like disorder (BDLD) with actual flaws (more than slight flaws but excessive preoccupation), BDLD without repetitive behaviours, body-focused repetitive behaviour disorder (eg. nail or lip biting, cheek chewing – patient tries to stop these actions), obsessional jealousy (non-delusional preoccupation with partner’s perceived infidelity that may be accompanied by repetitive behaviours and mental acts), shubo-kyofu (variant of taijin kyofusho – excessive fears of having a bodily deformity), koro (sudden fear that penis or vulva or nipples will recede into the body with or without a fatal outcome) and jikoshu-kyofu (olfactory reference syndrome: another variant of taijin kyofusho – fear of having offensive body odour).
Trauma and stressor-related disorders
Trauma and stressor-related disorders include reactive attachment disorder (child avoids comfort seeking and shows inadequate response to being comforted – seen in neglected children), disinhibited social engagement disorder (a neglected child is over familiar with unfamiliar adults), PTSD (specify if dissociation is present or there is a delay in onset – latter if full criteria not met for at least six months after event), acute stress disorder and adjustment disorders (anxiety, mixed anxiety-depression, conduct, mixtures of all foregoing).
Dissociative disorders
Dissociative disorders include dissociative identity disorder (described as a possession experience in some cultures), dissociative amnesia (with or without fugue), and depersonalisation/derealisation disorder.
Somatic symptom and related disorders
Somatic symptom and related disorders include somatic symptom disorder (with or without pain, persistence), illness anxiety disorder, conversion disorder (weakness or paralysis, abnormal movement, swallowing problems, speech symptoms, attacks/seizures, anaesthesia/sensory loss, special senses, mixed), psychological factors affecting other medical conditions and factitious disorder (imposed on self or others).
Feeding and eating disorders
Feeding and eating disorders include pica (in a child or an adult), rumination disorder, avoidant/restrictive food intake disorder (replaces feeding disorder of infancy/early childhood), anorexia nervosa (restricting or binge-eating/purging; BMI used to grade severity), bulimia nervosa (severity graded by weekly number of inappropriate compensatory behaviours), binge-eating disorder (patient binges at least weekly for three months and does not use inappropriate compensatory behaviours) and other specified feeding and eating disorders (includes purging disorder [patient wants to influence shape or weight but does not binge] and night eating syndrome [eats excessively at night after waking or shortly before retiring]).
Sleep-wake disorders
Sleep-wake disorders include insomnia, hypersomnolence, narcolepsy (include information on cataplexy, hypocretin status and other stated features), breathing-related sleep disorders such as obstructive sleep apnoea/hypopnoea, central sleep apnoea (CSA), Cheyne-Stokes breathing, CSA with opioid abuse, sleep-related hypoventilation, idiopathic hypoventilation, congenital central alveolar hypoventilation, comorbid sleep-related hypoventilation, circadian rhythm sleep-wake disorders (delayed or advanced phase, irregular and non-24-hour types) and shift work. Parasomnias include non-REM sleep arousal disorders, sleepwalking (with/without eating, sexual activity [sexsomnia]), sleep terror, nightmare, REM sleep behaviour disorder, restless legs and substance/medication-induced.
Sexual dysfunctions
Sexual dysfunctions include delayed ejaculation, erectile disorder, female orgasmic disorder, female sexual interest/arousal disorder, genito-pelvic pain/penetration disorder (combines vaginismus with dyspareunia), male hypoactive sexual desire disorder, premature/early ejaculation and substance/medication-induced sexual dysfunction. Gender dysphoria replaces gender identity disorder and focuses on dysphoria as the clinical problem rather than the identity as such; gender dysphoria refers to distress accompanying incongruity between experienced or expressed gender and assigned gender; one is asked to state the age group of the patient.
Disruptive disorders
Disruptive, impulse-control, and conduct disorders include oppositional defiant disorder (angry, irritable, touchy, easily annoyed, argumentative, vindictive; severity rated according to number of settings in which behaviour is manifested), intermittent explosive disorder (must be at least six years old), conduct disorder (state if onset in childhood or adolescence), antisocial personality disorder, pyromania and kleptomania. This group of disorders manifests in behaviours that violate the rights of others and/or bring the individual into significant conflict with societal norms or authority figures. Different component disorders affect emotional and behavioural regulation differently. Many defining symptoms can occur in typically developing individuals so one must know what is normative.
Substance-related disorders
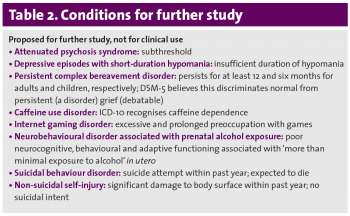
Substance-related and addictive disorders include substance use and substance-induced disorders: alcohol, caffeine, cannabis, phencyclidine, other hallucinogen, hallucinogen persisting perception disorder, inhalant, opioid, sedative/hypnotic/anxiolytic, stimulant, tobacco and other substances (specify intoxication, withdrawal). Pathological gambling is included here. Internet gaming and sex/exercise/shopping addiction are not included but not enough is known about them.
Neurocognitive disorders
Neurocognitive disorders include dementia and amnestic disorder. Objective tests should be interpreted carefully, eg. a poor result may reflect the normal state of the patient. Delirium (state known cause/s, duration, hyperactive or hypoactive or mixed) and major and mild neurocognitive disorders (Alzheimer’s, frontotemporal, Lewy body, vascular, trauma, HIV, prion, Parkinson’s disease, Huntington’s disease, other/multiple causes) are found in this chapter. Mild cases were subsumed under “cognitive disorders not otherwise specified” in DSM-IV. In mild cases patients are able to manage their affairs, although with greater effort; compensatory strategies or accommodation may be required. One must outrule delirium and depression. Boundaries between normal and poor neurocognitive functioning are inherently arbitrary. Both history and objective assessment are required.
Other mental disorders
Other mental disorders include those due to a specified or unspecified medical condition. Medication-induced movement disorders and other adverse effects of medication include, for example, postural tremor, tardive dyskinesia and antidepressant discontinuation syndrome. Other conditions that may be a focus of clinical attention are not mental disorders but are included to draw attention to them – they cover family issues, primary support group, abuse/neglect, spouse/partner issues, education/occupation, housing and economic, social environment (includes stigma), crime/legal system and other (including non-adherence, availability of services, overweight/obesity, malingering and borderline intellectual functioning).
Cultural formulation involves a systematic assessment of cultural identity (patient’s reference groups), a cultural conceptualisation of distress (eg. explanatory models), psychosocial stressors and cultural features of vulnerability/resilience (environment, religion, supports, etc), cultural features of relationship between individual and clinician (such as language, experience of racism, etc) and a synthesis of the foregoing under “overall cultural assessment”. The Cultural Formulation Interview includes 16 questions covering items such as values, current social context and influence of others.
Personality disorders
The alternative DSM-5 model for personality disorders focuses on impaired personality functioning (disturbed self and interpersonal functioning) and abnormal personality traits (five broad trait domains containing 25 specific trait facets). It can be used to derive antisocial, avoidant, borderline, narcissistic, obsessive-compulsive and schizotypal personality disorders. It can also diagnose what amounts to non-specified (mixed) personality disorder. The model also looks at pervasiveness/stability and differential diagnosis.
 (click to enlarge)
(click to enlarge)

 (click to enlarge)
(click to enlarge)