NUTRITION
Assessing and managing micronutrient deficiency in a paediatric patient
Deficiency of iron, iodine and vitamin A are widespread globally, with particularly detrimental effects for infants and children
November 23, 2019
-
With improved overall nutrition and food availability, these have been observed less and less in the developed world.1
However, it is still common in many populations, particularly children, where there are high demands for growth and development. In Ireland, one in 10 toddlers has inadequate intakes.2 Inadequate vitamin A and D intakes have also been highlighted in our toddler population.2 Children with autism often have particularly restricted diets and may be at greater risk of micronutrient deficiency. Interestingly, recent papers from the US and Ireland have highlighted vitamin C deficiency3 and concomitant vitamin A and D deficiency4 respectively in children with autism.
Micronutrient deficiencies can occur in all settings and the registered dietitian (RD) is an important member of the team when it comes to assessing, intervening and monitoring the patient. In this piece, the case of a child with an extremely restricted oral diet presenting with micronutrient deficiency is discussed.
Case
Client history: Suspected autistic spectrum disorder, global developmental delay, non-verbal and poor sight.
Medical investigations and observations: The child presented at three years old with profound iron deficiency anaemia. The child had an extremely restricted diet and was referred to dietetics. She was not linked with community services at presentation. The child was also referred to dentistry.
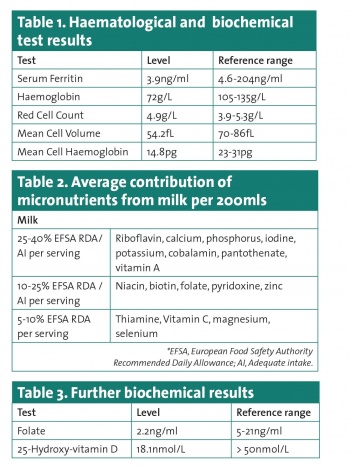
Biochemistry/Lab values: Hypochromic, microcytic anaemia was present with low serum ferritin. Serum Iron was also low. C-reactive protein (CRP) was within reference range (see Table 1).
Medications and prescribed nutrition: The child was started on 5ml of ferrous fumarate once daily, equal to 45mg of elemental iron or ~3mg/kg per day. No other medications or supplements were used.
Nutrition-focused physical findings: The patient presented with no overt symptoms of deficiency (eg. nail ridges, koilonychia, glossitis, stomatitis). Poor dentition was noted with significant plague build-up. No lower gastrointestinal issues were reported at baseline.
Anthropometry: Weight and height on WHO-UK centile charts were on the 98% and 91% respectively and no historical growth issues were evident
Nutrition-related history: (Summary) Intake was high in sugar and refined carbohydrate. Based on growth, overall energy need was met along with sufficient protein. Most importantly, the diet lacked almost any source of iron or copper. Calcium and tannin intake were potentially exacerbating inadequate iron intake. Milk alone is, however, a remarkably complete food providing significant contributions of a host of micronutrients (see Table 2). Dietary analysis using food composition data showed that significant additional contributions of other nutrients not provided by dairy were supplied by popcorn, waffles and crisps such as thiamine, vitamin C, E and K, zinc and manganese – 50-100% European Food Safety Authority (EFSA) recommended daily allowances (RDAs)/adequate intakes (AIs).
Given suboptimal intakes, serum vitamin D, folate, selenium and copper were analysed. Vitamin A was analysed to rule out any contribution to existing visual impairment. It is important to note that serum copper and selenium are not ideal markers of status, but are used clinically.5 See Table 3 for further biochemical results.
 (click to enlarge)
(click to enlarge)
