MENTAL HEALTH
Attitudes towards mental illness among Irish medical professionals
A survey of medical professionals showed that negative attitudes towards mental illness are particularly high among medical students
December 8, 2017
-
Stigma surrounding mental health has long been noted to be extremely high in the general population.1 Indeed, media and narrative including books, plays and films have long established a violent and frightening portrayal of patients with mental illness.2 It is therefore little wonder that stigma in the general population is still at high levels.3
Research across multiple continents has shown repeatedly that stigma exists among medical professionals.4 Some work has suggested that those working in mental health settings may have less negative attitudes towards people with mental illness than do general healthcare providers.5 There is an assumption of a clear link between negative attitudes and discriminatory professional behaviours towards persons with mental illness.6,7 This assumption has rarely been examined, hence the reason to question the assumed link between negative attitudes and negative professional behaviours.8
First and foremost, attitude-behaviour relationships are generally weak, regardless of subject matter and settings.9 Secondly, behaviour of professionals towards patients is likely to be influenced by multiple situational factors, including adherence to professional ethics, clinical role/setting and patient characteristics. On the other hand, discriminatory practices by clinicians towards persons with mental illness are common.10
Schulze also showed that negative views of medical professionals towards psychiatry can serve to propagate stigma and indeed reinforce patient’s reluctance to seek treatment.4 Furthermore, stigma leads to diagnostic overshadowing and an overall poorer level of care for physical health complaints for patients with mental illness.11
Stigmatising attitudes may inhibit individuals with a mental disorder to seek help, which directly creates barriers to their successful reintegration into society while increasing their psychological distress.12
Aims of the study
This study aimed to ascertain attitudes among medical professionals in Ireland towards mental illness. The authors also explored whether there was a difference in stigma towards mental illness depending on area of work (ie. hospital versus general practice) and level of training in medicine (ie. medical student versus trained professionals).
Methods
A representative sample of medical professionals was chosen on which to focus the study. Contact information was obtained from the Irish Medical Directory. A total of 450 medical doctors, including general practitioners and hospital doctors, were included, and a further 150 medical students and interns were also surveyed. As this was a survey, involving trained and trainee medical professionals, the authors felt that ethical approval was not required.
The authors surveyed various medical professionals using a questionnaire based on a validated tool to ascertain stigma towards mental illness, called MICA V4 (Mental Illness Clinicians Attitude, version 4) scale.13 The MICA scale is a self-administered fast tool, which can be completed in approximately five minutes. It is a 16-item, Likert scale type questionnaire with Cronbach’s alpha value of 0.72, indicating good reliability. It also showed good validity and acceptability as a tool. A person’s MICA score is the sum of the scores for the individual items. Items 3,9,10,11,12 and 16 are scored as follows: strongly agree = 1, agree = 2, somewhat agree = 3, somewhat disagree = 4, disagree = 5, strongly disagree = 6. All other items (1,2,4,5,6,7,8,13,14,15) are reverse scored. A high overall score indicates a more negative (stigmatising) attitude.
The authors created an anonymous e-survey from the questionnaire, using ‘survey monkey’, which was circulated to a representative sample of professionals belonging to various disciplines in medicine. It was also circulated to GPs and medical students including interns. Survey monkey was used to provide ease of distribution and collection of data.
The participants were contacted by email and provided with a detailed description of the purpose of the survey. The anonymity of their responses was assured. They were sent a link to the survey and asked to complete it online. A total of two reminders, two weeks apart, were sent to all the professionals, after which the survey was closed after that. The results were collated and analysed using SPSS.
Results
Of the 600 questionnaires distributed, 152 individuals responded, which amounts to a response rate of 25.3%. This is considered an adequate response rate for online surveys14 however, we cannot rule out the possibility of a selection bias. Of these, 126 questionnaires had sufficient data for analysis. The specialty was available for 120 individuals and the breakdown was: medical students and interns (n = 42), general practitioners (n = 53) and hospital doctors (combination of physicians, surgeons and anaesthetists, n = 25).
Individual stigma score was calculated for each responder. The individual stigma scores displayed a normal distribution across the entire sample. Results were then stratified and analysed according to specialty, age and gender. Independent sample t-tests were used to compare means between groups and the results were as follows.
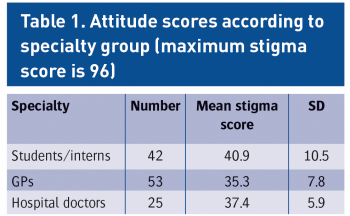
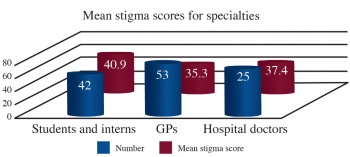
Specialty groups
As evident from Table 1, there was an interesting trend observed in the stigma scores between the different professional groups. Medical students and intern group scored higher in the mean stigma score and this difference was statistically significant when compared to the GPs [medical students/interns (n = 42, mean stigma score = 40.9, SD = 10.5) versus GPs (n = 53, mean stigma score = 35.3, SD = 7.8) (t = 2.96, p = 0.004)].
When medical students and interns were compared with hospital doctors, the former group still had higher stigma scores but the difference was not statistically different [medical students/interns (n = 42, mean stigma score = 40.9, SD = 10.5) versus hospital doctors (n = 25, mean stigma score = 37.4, SD = 5.9) (t = 1.76, p = 0.084)].
The scores were even more comparable when we looked at the two groups of GPs and hospital doctors. The latter group had slightly higher mean stigma scores but there was no statistical difference between them. [GPs (n = 53, mean = 35.3, SD = 7.8) versus hospital doctors (n = 25, mean = 37.4, SD = 5.9) (t = -1.15, p = 0.252)].
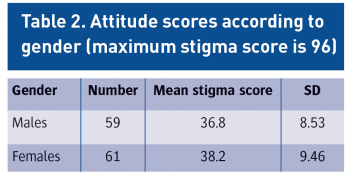
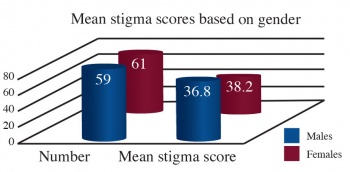
Gender
Gender was available for 120 individuals and was divided as follows: males n = 59 (49.2%) and females n = 61 (50.8%). There was no significant difference between gender groups: [males (n = 59, mean = 36.8, SD = 8.53) as compared to females (n =61, mean = 38.2, SD = 9.46), t = -0.84, p = 0.402.]
Age groups
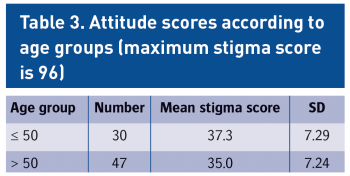
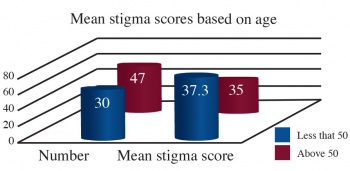
There was an apparent trend noticed in mean stigma scores in the different age groups, with the scores seemingly going down with advancing age (see Figure 3). The highest stigma score was in the youngest age group of 21-30 years with the least being in the 51-60 age group. Even though there was this trend, no statistically significant difference was evident between the age groups.
For ease of analysis the age groups were divided into two, less than or equal to 50 and above 50. The results were as follows: 50 years or less (n = 30, mean = 37.3, SD = 7.29) versus more than 50 years (n = 47, mean = 35.0, SD = 7.24), t = 1.37, p = 0.175.
 (click to enlarge)
(click to enlarge)

 (click to enlarge)
(click to enlarge)
 (click to enlarge)
(click to enlarge)
 (click to enlarge)
(click to enlarge)
 (click to enlarge)
(click to enlarge)
 (click to enlarge)
(click to enlarge)