CARDIOLOGY AND VASCULAR
MENTAL HEALTH
DIABETES
ENDOCRINOLOGY
NEUROLOGY
Communicating hydrocephalus
The correct steps to take in the diagnosis and management of hydrocephalus
December 2, 2013
-
Hydrocephalus can be defined broadly as a disturbance of formation, flow or absorption of cerebrospinal fluid (CSF) that leads to an increase in the volume occupied by this fluid in the central nervous system (CNS). This condition also could be termed a hydrodynamic disorder of CSF. Acute hydrocephalus occurs over days, subacute hydrocephalus occurs over weeks and chronic hydrocephalus occurs over months or years.
Conditions such as cerebral atrophy and focal destructive lesions also lead to an abnormal increase of CSF in CNS. In these situations, loss of cerebral tissue leaves a vacant space that is filled passively with CSF. Such conditions are not the result of a hydrodynamic disorder and therefore are not classified as hydrocephalus. An older misnomer used to describe these conditions was hydrocephalus ex vacuo.
Case report 1
A 63-year-old male who has a history of sero-positive rheumatoid arthritis (RA) on sulfapyrizine, was brought to the emergency department (ED) early in the morning unresponsive. He was found in bed at home by his relative who noticed that his breathing was getting laboured and noisy. He was also found incontinent of urine with vomiting by his bed sheet. There was no seizure witnessed.
He went to his bed normally the night before with no prior history of acute illnesses apart from his usual flares of rheumatic joint pains which are controlled with oral and parenteral non-steroidal anti-inflammatory drugs (NSAIDs) by his GP, although later a friend of the patient stated that he was texting him misspelled messages for the past two days, however, he wasn’t particularly confused or showing any behavioural change. His BP was 208/143 at scene by the ambulance crew. In the ED he was febrile and comatose (GCS 6/15) with no spontaneous limb movements. The initial CT brain was reported as communicating hydrocephalus which was likely old with no other findings (see Figure 1).
He was mechanically ventilated and remained in the intensive care unit (ICU) for the following 14 days. Investigations showed neutrophil leucocytosis and raised inflammatory markers in his blood. Meningoencephalitis was the working diagnosis from the beginning and he was covered with antimicrobial and antiviral from day one. His CSF analysis showed 35 WBC per/ul (95% lymphocytes), glucose of 3.5mmol (plasma 7.6mmol) and protein of 0.74g/L. Extensive microbiological analysis (including polymerase chain reaction [PCR]) failed to identify any organisms. The repeat CT brain three days later showed areas of low densities at right internal capsule and right temporo-parietal lobe, which are new since the first scan (see Figure 2) and which were suggestive of infarcts, and stroke was a possibility at that stage and was discussed with his family. The course of management, however, remained the same (completed full course of parenteral antibacterial and antiviral) and these areas totally disappeared in the later scans with no adequate explanation to their nature and implication.
He subsequently improved with supportive measures: hydration and nutrition through nasogastric tube (NGT) feeding. He also retained his spontaneous breathing. He is currently maintaining adequate oral intake, having slurred speech and being incontinent of urine and faeces. He is fully dependent and requires full assistance on daily living activities due to residual weakness of all his limbs (grade 3/5 upper limbs, 2/5 lower limbs) and is awaiting a bed in the National Rehabilitation Centre.
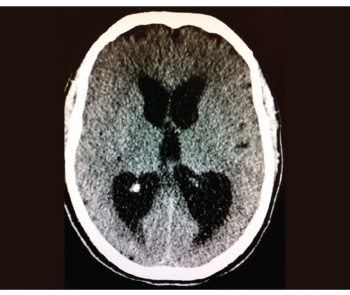 Figure 1. The initial CT brain at presentation showing the communicating hydrocephalus(click to enlarge)
Figure 1. The initial CT brain at presentation showing the communicating hydrocephalus(click to enlarge)

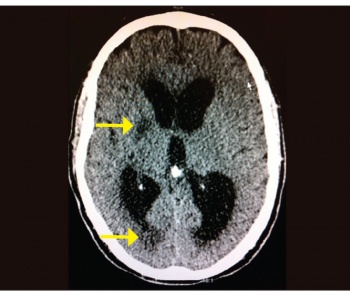 Figure 2. The repeat CT showing the new areas of low attenuation (arrowed) which were thought to be infarctions but disappeared eventually(click to enlarge)
Figure 2. The repeat CT showing the new areas of low attenuation (arrowed) which were thought to be infarctions but disappeared eventually(click to enlarge)
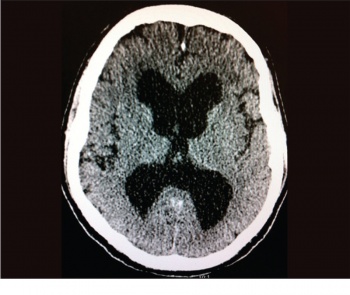 Figure 3. CT brain showing gross communicating hydrocephalus(click to enlarge)
Figure 3. CT brain showing gross communicating hydrocephalus(click to enlarge)
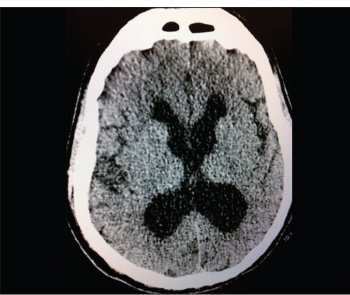 Figure 4. The CT brain following removal of 50ml CSF. Note the reduction in ventricular size that did not correlate with clinical improvement(click to enlarge)
Figure 4. The CT brain following removal of 50ml CSF. Note the reduction in ventricular size that did not correlate with clinical improvement(click to enlarge)