MENTAL HEALTH
Diagnosis and length of stay at an acute psychiatric unit
Examination of the length of stay following psychiatric admission, with a particular focus on the relationship, if any, between diagnosis and length of stay
November 10, 2017
-
While there has been increased research into many aspects of psychiatric admission in Ireland over recent years, relatively little is known about correlates and determinants of length of stay for those admitted. This paper looks in more depth at length of stay following psychiatric admission, with particular focus on the relationship, if any, between diagnosis and length of stay.
To this end, we studied all admissions (voluntary and involuntary) to an acute psychiatric unit in south west Dublin between January 1, 2014 and June 30, 2015, and compared it with national data. We found that longer length of inpatient psychiatric stay was independently associated with involuntary status and increased age, and was not independently associated with gender, diagnosis, marital status or occupational status.
Despite these associations, most of the variance in length of stay (92%) remains unexplained by the factors examined in this study, suggesting that other variables, yet to be identified, play significant roles in determining duration of inpatient psychiatric admission.
Introduction
In 2015 there were 17,860 admissions to inpatient psychiatric facilities in Ireland, of which 2,144 were involuntary admissions under the Mental Health Act 2001.1 While recent years have seen increased research into both voluntary and involuntary admission in Ireland,2,3 there are still significant gaps in the literature especially in relation to specific topics such as length of stay (duration of admission).
We recently studied patterns of voluntary and involuntary admission in south west Dublin over 18 months in 2014/2015.4 We found that rates of involuntary admission had increased in this area compared to previous years but that the overall admission rate was still lower than the national rate.
We also found that mean length of stay for involuntary patients (59.4 days, standard deviation [SD] 98.0) was substantially longer than that for voluntary patients (18.9 days, SD 38.4; p < 0.001).
The purposes of this paper were to look in more depth at length of stay among all psychiatry inpatients in this area, voluntary and involuntary, with particular focus on the relationship, if any, between diagnosis and length of stay, and to compare with national data published by the Health Research Board, especially in terms of diagnosis.5
Methods
We studied all admissions to the acute psychiatric unit in Tallaght Hospital, Dublin (south west Dublin) between January 1, 2014 and June 30, 2015. For each patient, we recorded a range of details including gender, date of birth, marital status, occupational status, date of admission, admission status (voluntary or involuntary for all or part of the admission), date of discharge, and clinical discharge diagnosis using the International Classification of Diseases, Volume 10.6
This study was approved by the Joint Research Ethics Committee of St James’s Hospital and Tallaght Hospital and performed in accordance with the Declaration of Helsinki7 and Data Protection Guidelines on Research in the Health Sector.8
We stored and analysed data using IBM Statistical Package for the Social Sciences (SPSS) Statistics (Version 24). Data were normally distributed except where non-parametric bi-variable tests are specified. For multi-variable analysis, we generated a multi-variable linear regression model with length of stay as the dependent variable. Gender, age, marital status, occupational status, admission status (voluntary or involuntary) and diagnosis were entered as independent variables.
We tested the regression model for multicollinearity, which is when one or more variables are so closely related to each other that the model cannot reliably distinguish the independent effects of each. To test this, we calculated a ‘tolerance value’ for each independent variable; tolerance values below 0.25 indicate possible multicollinearity, and tolerance values below 0.10 indicate significant problems with multicollinearity.9
Results
We have already reported that during the 18-month period studied there were 948 admissions of which 13.5% were involuntary.4 Over one-third of patients in the study area (39.2%) were discharged within one week and over three quarters (76.1%) were discharged within one month;4 these were slightly higher than comparable national figures (29.9% and 67.0% respectively).5 The present study focuses more closely on the relationship, if any, between length of stay and various other potentially relevant variables, such as diagnosis, gender, age, marital status and occupational status.
We found that length of stay did not differ between men (median duration of admission: 11 days; inter-quartile range: 3-28) and women (median duration of admission: 9 days; inter-quartile range: 3-24; Mann-Whitney U: 117, 861.5, p = 0.163). Length of stay correlated positively with age (Spearman’s rho: 0.171, p < 0.001) but was unrelated to marital status (independent-samples Kruskal-Wallis test: 1.793, p = 0.774) or occupational status (independent-samples Kruskal-Wallis test: 4.826, p = 0.185).
Table 1 presents the relationship between diagnosis and length of stay both in the study area and nationally. There are notable similarities between the study area and national data: 58.3% of patients with schizophrenia and 73.1% with affective disorders were discharged within four weeks in the study area, compared to 59.0% and 65.4% nationally.5 There are also contrasts: 65.8% of patients with personality disorders and 69.0% with drug disorders (other than alcohol) were discharged within one week in the study area, compared to 49.5% and 51.4% nationally.5
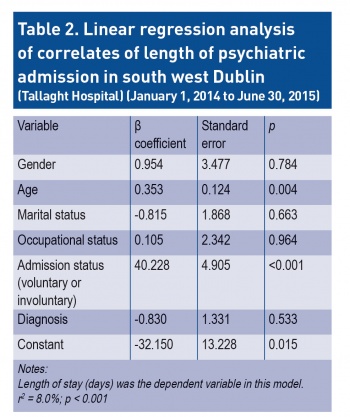
On multi-variable linear regression analysis, with length of stay as the dependent variable, longer length of stay was significantly associated with involuntary admission status and older age (see Table 2). We calculated a ‘tolerance value’ for each independent variable in the model and all tolerance values were greater than 0.25 indicating no significant problems with multicollinearity
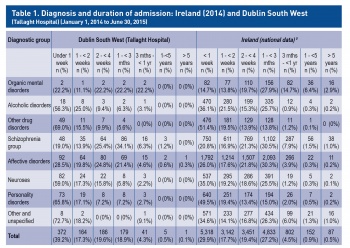 (click to enlarge)
(click to enlarge)

 (click to enlarge)
(click to enlarge)