GASTROENTEROLOGY
Haemobilia: symptoms, diagnosis and treatment
Haemobilia, a rare cause of upper gastrointestinal (GI) bleeding following liver biopsy
February 10, 2014
-
A male in his early 70s who has a background history of hypertension, renal cell carcinoma (RCC) post-left nephrectomy five years ago, was referred to the gastroenterology clinic for evaluation of mildly persistently elevated liver enzymes.
Case report
Initial work-up, including hepatitis profile and autoimmune screen, was negative. His liver functions including bilirubin, albumin and international normalised ratio (INR) were normal. Subsequently, he was scheduled for percutaneous liver biopsy which was done under ultrasound guidance. Two days after the biopsy he developed right upper quadrant abdominal pain, jaundice and black stool and so was admitted to the hospital. His haemoglobin dropped to 7.5 so he was transfused with three units of red blood cells. Abdominal ultrasound showed blood within the biliary system. He was managed conservatively and the haemoglobin remained stable, the abdominal pain resolved and he was discharged home. Two days later he was readmitted with worsening abdominal pain.
Upper GI endoscopy done during this admission showed blood within the distal stomach, and more fresh blood within D1 and D2 with blood coming from the ampulla of Vater. This confirmed the diagnosis of haemobilia. The liver biopsy was reported as mild inflammation and fibrosis without significant cirrhosis.
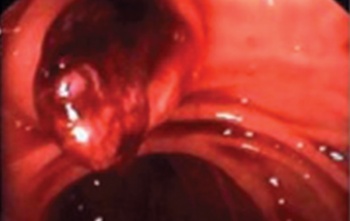 Figure 1. Blood coming from ampulla of Vater at upper GI endoscopy (click to enlarge)
Figure 1. Blood coming from ampulla of Vater at upper GI endoscopy (click to enlarge)

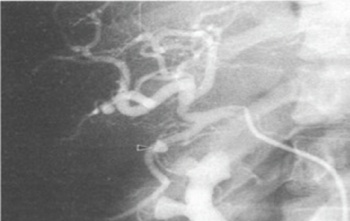 Figure 2. Blood within the biliary ducts (click to enlarge)
Figure 2. Blood within the biliary ducts (click to enlarge)