MENTAL HEALTH
Improving the quality of discharge summaries
An audit of the impact of educational intervention on the quality of discharge summaries in an inpatient psychiatric unit in a general hospital
September 1, 2015
-
Traditionally communication between primary care and hospitals has been deemed suboptimal. The evolution of psychiatric services towards a community model of care warrants an improvement in the communication between the psychiatric services and primary care providers. There is evidence to suggest that with auditing, the quality of discharge summaries can be improved.
Aim
Our aim was to examine and attempt to improve the recording of information within psychiatric discharge summaries in an adult psychiatry department, by means of audit and feedback.
Introduction
The discharge summary is an important communication tool which aims to summarise the therapeutic and other significant events during inpatient stay. It provides concise details of reasons leading to admission, diagnosis, investigations, etc, and is also helpful as a record of responses to different therapeutic interventions. It can be referred to years later to provide a quick summary of an inpatient stay.
The discharge summary is useful for primary care providers to continue on the treatment strategies planned during admission. Comprehensive and timely communication between hospitals and general practitioners (GPs) is essential to ensure safe transition from the hospital back to the community. There is evidence to suggest that this may not happen on many occasions.1 A high-quality discharge summary provided to the appropriate care provider at the right time can potentially reduce adverse events after discharge, decrease healthcare costs, and promote positive outcomes for patients.2,3 On the other hand, poor information transfer at discharge does appear to increase the likelihood of readmission.4 Research suggests that GPs attribute more than one-third of post-discharge adverse events to unsatisfactory information transfer.5
The purpose of the discharge summary is particularly important in the context of content and timing. In a survey of the views of GPs on psychiatric discharge summaries the top five headings identified in terms of importance were: admission and discharge dates, diagnosis, medications on discharge, community key worker and date of follow-up.6 This is understandable since GPs are mainly concerned about implementing the post discharge care plans.
Our study was undertaken in an acute adult psychiatric setting in order to analyse the quality of discharge summaries against local guidelines issued by Kerry Mental Health Services. These guidelines are based on Mental Health Commission Code of Practice on Admission, Transfer and Discharge to and from an Approved Centre.7 We also aimed to evaluate the satisfaction of GPs receiving these documents. We intended to improve the quality of these documents and resultant satisfaction gradient of the catchment area GPs by a brief educational intervention aimed at the non-consultant hospital doctors (NCHDs) responsible for completing these documents.
Methods
The study was conducted in an inpatient psychiatric unit in a general hospital that is divided into two wards, which have 19 and 23 beds respectively. Discharge summaries are prepared by the psychiatric registrars and senior house officers, typed by secretaries and sent to the patient’s GP, with copies filed to the respective case notes.
The aim of the audit was to assess the standards of discharge summaries against local guidelines, and to examine whether feedback and educational intervention resulted in any improvement in same. The local guidelines state that the following information should be included:
- Date of admission and discharge
- Status of admission
- Presenting complaints
- Mental state and physical examination on admission
- Progress and treatment given
- Results of investigations
- Discharge diagnosis with International Classification of Disease (ICD) code
- Medications on discharge
- Follow up arrangements.
Moreover, the guidelines also state that letters should be typed and filed with case notes within seven days of discharge. In addition to the analysis of the summaries, the authors also sent out purpose designed, face validated, Likert type questionnaires to GPs, the purpose of which was to elicit their opinion on attributes pertaining to the discharge summaries which they received from the KGH psychiatric unit. GPs were explicitly asked for their opinion on the following attributes of the summaries:
- Timeliness
- Information provided helpful in patient management
- If more information was needed in the summaries
- If they thought the summaries were too cumbersome
- If they felt relevant information was captured in the summaries
- If they were happy with the overall quality of the summaries.
The overall aim of the study (and the aim of contacting GPs) was to examine whether auditing and feedback coupled with an educational intervention would improve discharge summaries and increase GPs’ satisfaction.
Results
The summaries from case notes of 44 patients who were discharged from the acute adult psychiatric wards, over a period of three months, were obtained. Data was collected while leaving enough time for the discharge summaries to be filed in the respective case notes. In the next intake of NCHDs in the psychiatry department, the new registrars and senior house officers were briefed on the audit by the lead author. This included feedback of the results from the first cycle of the audit, focusing mainly on the areas for improvement, along with reiteration of the local guidelines. Clinicians were encouraged to adhere to these guidelines in an attempt to improve quality of discharge summaries.
The cycle was then repeated for another three months with 48 summaries analysed. All the discharge summaries were evaluated using a questionnaire which was devised following above mentioned guidelines. This questionnaire was face validated by the authors and other consultants working in the hospital. Data was analysed using SPSS version 17.
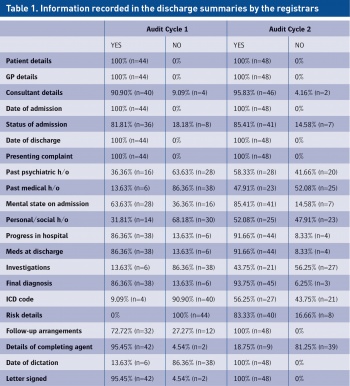
Table 1 shows the comparison of the information recorded in the discharge summaries by the registrars between cycle one and two. There were significant changes in ‘Past med history’ Chi Sq χ = 0.00 and ‘Past psych history’ Chi Sq χ = 0.03 between cycle one and cycle two.
In addition, reporting information such as the ‘ICD code’ χ = 0.00, the ‘Mental state’ χ = 0.01, ‘Personal/social history’ χ = 0.04 and ‘Investigation carried out’ χ = 0.02, were significant between both audit cycles. Not surprisingly, no significant differences regarding changes in reporting ‘Consultant details’ χ = 0.29, ‘Progress in hospital’ χ = 0.51, ‘Final diagnosis’ were found between cycles.
Following consultation with the GPs we compared their ratings of discharge summaries between cycles one and two (see Table 2).
Encouragingly there were some significant changes between both cycles. GPs’ ratings of ‘Happiness with time-line’ Z = 0.03 and ‘Relevant information included’ Z = 0.02 yielded significant results between cycles, while, ‘Information helpful in management of patients’ Z = 0.22, ‘Would like more info on summaries’ Z = 0.72, ‘Summaries were too cumbersome’ Z = 0.69, and ‘Happy with overall quality of summaries’ Z = 0.84 were not significant between audit cycles. These results are encouraging because even though GPs’ responses suggest that we did improve the timeliness of our discharge summaries and included more clinically relevant information, they always felt that discharge summaries helped them in the management of their patients. GPs were also happy with the content of the information in the summaries and wouldn’t like them to be more cumbersome.
The results also suggest that even though a brief educational intervention can improve the quality of the discharge summaries, it does not necessarily translate into improved satisfaction for the GPs with these documents. Another way of looking at this would be that GPs were always happy enough with these documents.
 (click to enlarge)
(click to enlarge)
