WOMEN’S HEALTH
Management of mastocytosis throughout pregnancy
A clear management plan for the antenatal period, labour and postnatal period should be devised for the patient
June 24, 2016
-
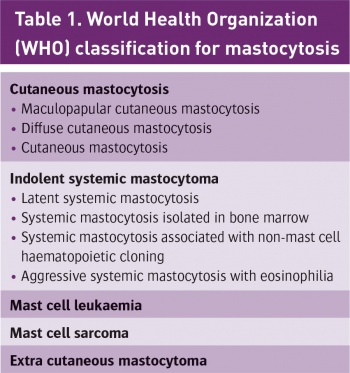
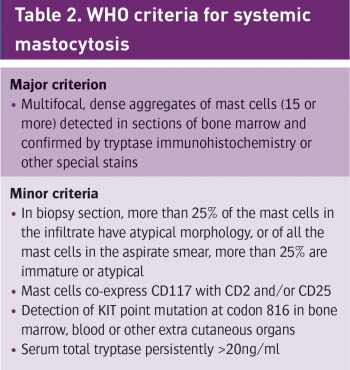
Mastocytosis is a rare disease, characterised by pathologic increase in mast cells in cutaneous tissue and extra cutaneous organs such as the bone marrow, liver, spleen and lymph nodes. It comprises many different clinical presentations varying from indolent cutaneous forms to malignant and systemic conditions. Episodes of life-threatening anaphylaxis are a recognised feature of the disease. This case report highlights the management of cutaneous and systemic mastocytosis in pregnancy.
A 28-year-old primigravida booked for antenatal care in the hospital at 28 weeks gestation. She had no significant family history. She had recently been diagnosed with cutaneous mastocytosis. Mastocytosis work up was performed because she collapsed twice while hiking in mountains seven years ago. She had no apparent systemic reaction, however she was hospitalised and required epinephrine following the first event. There were no further events for seven years.
She gave a history of a cutaneous rash for at least 10 years, small pinkish light brown papules which become erythematous with irritation or sun exposure. She also had a history of intermittent flushing and urticaria. Her diagnosis was based on pathological examination of a skin biopsy which demonstrated a mast cell infiltrate in the upper dermis consistent with urticaria pigmentosa. She also had elevated tryptase level, a marker of mast cell degranulation released in parallel with histamine. She had negative CKIT D816V mutation, which was reassuring as far as risk to future offspring was concerned.
Of note, most forms of mastocytosis are caused by a mutation of the KIT gene on the 4q12 chromosome – a mutation which increases cellular reproduction. Mastocytosis can be associated with allergic and anaphylactic reaction; consequently she has been prescribed an EpiPen in case of an anaphylaxis by her physicians.
When the woman booked for antenatal care she was referred to a high risk antenatal clinic, which included regular foetal biometry assessment, and attendance at specialised anaesthetic and haematology clinics. Her case was discussed at our monthly multidisciplinary meeting (also attended by lead hospital pharmacist) and at 36 weeks gestation a final plan of care was devised and circulated to relevant personnel. The team reviewed all available data and agreed that when she presented in labour, she should receive 100mg IV hydrocortisone (with consideration of six hourly hydrocortisone also) and should be given PO antihistamine, eg. chlorphenamine 10mg, IV. A list of histamine releasing drugs to be avoided included morphine, codeine, aspirin, suxamethonium, atracurium and rocuronium. Non-steroidal drugs to be avoided included diclofenac sodium (Difene), ibuprofen and mefenamic acid (Ponstan). Drugs which were considered safe for use included propofol, ketamine, fentanyl, sevoflurane and paracetamol. Early epidural was recommended in order to avoid a general anaesthetic. Consultant involvement at all times was also recommended. It was decided to involve a consultant anaesthetist if the woman required a cesarean section and to be transferred to high dependency unit postpartum. The plan for post-operative pain was for an epidural infusion for 24 hours and fentanyl via patient controlled analgesia to help control her pain. In the case of postpartum haemorrhage oxytocin was to be used. If there was any evidence of infection clindamycin and ciprofloxacin were considered safe to be used, however vancomycin was to be avoided. There was also a consideration for the use of high sensitivity gloves. Most importantly, it was agreed that adrenaline should be readily available. If she became hypotensive following epidural administration epinephrine should be administered.
Ultimately spontaneous labour occurred at 40+4 weeks and she used entonox and received an early epidural as planned. A female baby weighing 4.18kg was delivered by spontaneous vaginal delivery with a second degree tear occurring, which was sutured. She was transferred to the high dependency unit postpartum. Neither local anaesthetic agents nor antibiotic agents caused any reaction. The postpartum period was uneventful.
 (click to enlarge)
(click to enlarge)

 (click to enlarge)
(click to enlarge)
 Figure 1. Cutaneous mastocytosis furticaria pigmentosal(click to enlarge)
Figure 1. Cutaneous mastocytosis furticaria pigmentosal(click to enlarge)