WOMEN’S HEALTH
Recurrent ectopic pregnancy in tubal stump after previous salpingectomy
A rare case of ipsilateral ectopic pregnancy after salpingectomy discussed by a team from Portiuncula University Hospital
December 7, 2019
-
Ipsilateral ectopic pregnancy after total or partial salpingectomy is a rare occurrence with very few cases reported in literature. We report a case where the spontaneous ectopic occurred in stump of the previously removed tube. We have explained possible hypothesis for such recurrence and surgical techniques which could possibly avoid such recurrence have been suggested.
Ectopic pregnancy
Ectopic pregnancy is defined as pregnancy which implants outside the uterine cavity. More than 90% of ectopic pregnancy occur in one of the fallopian tubes. The incidence of ectopic pregnancy is around 1-2%. The incidence of recurrence is 15% after one and 30% after two ectopic pregnancies.1,2 However, the exact incidence of ectopic pregnancy in remnant stump following salpingectomy is not known.
Case report
A 35-year-old woman, para 0+2, presented to the emergency department with sudden onset of severe lower abdominal pain, vomiting and bilateral shoulder tip pain. The patient had been on her third day of her menstrual cycle, had regular periods and was not on contraception. Her pulse rate was 130 and blood pressure was 84/51mmHg at time of presentation. On examination guarding was noted all over her abdomen with more tenderness in the right iliac fossa. Bloods were taken and fluid resuscitation was commenced. The patient was unable to produce urine therefore an urgent serum beta-hCG was requested. She had had a first trimester miscarriage in her first pregnancy and had a right salpingectomy for ruptured ectopic pregnancy around 18 months previously in her second pregnancy.
Serum beta-hCG result was 5,574mIU/mL and haemoglobin (Hb) level was 8.3mmol/L. An urgent ultrasound by the gynaecology team showed her abdomen was full of echogenic fluid and no evidence of intrauterine gestational sac. A working diagnosis of ruptured ectopic pregnancy was made and patient was taken to theatre for laparoscopy.
After arrival in theatre routine three-port laparoscopy was done with entry via umbilical incision using Verres needle. Abdomen contained a copious amount of blood, which was suctioned rapidly. The left tube and ovary were noted to be normal.
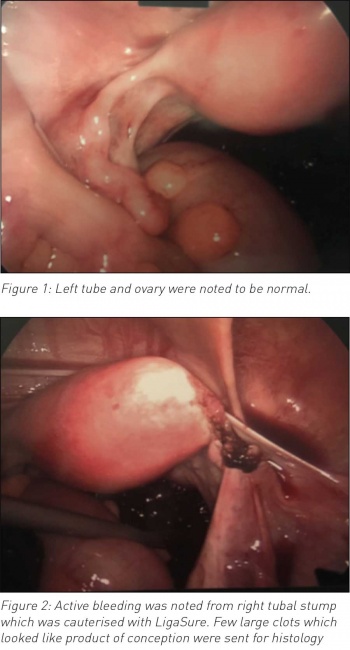 (click to enlarge)
(click to enlarge)
