WOMEN’S HEALTH
Successful treatment of uterine arteriovenous malformation
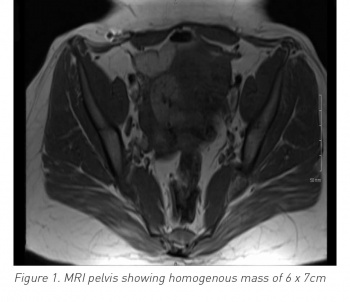
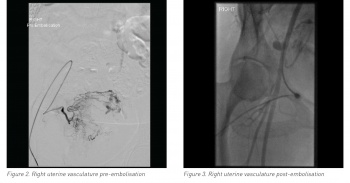
An obstetrics and gynaecology team report on a rare case of uterine arteriovenous malformation, successfully treated with bilateral uterine artery embolisation
January 24, 2020
-
Uterine arteriovenous malformation (AVM) is defined as abnormal and nonfunctional connections between the uterine arteries and veins. Although rare, it is a potentially life-threatening condition. Fewer than 100 cases are reported in existing literature and include patients who presented with per vaginam (PV) bleeding, often mild to moderate, but sometimes life-threatening. It is likely to occur during a woman’s reproductive years and treatment depends on signs and symptoms, as well as future fertility requirements. If symptoms are not improved with conservative treatment, uterine artery embolisation is required to avoid the need for a hysterectomy.
This report looks at a case of acquired uterine AVM, confirmed by angiography, which was successfully treated with bilateral uterine artery embolisation.
Introduction
There are two types of AVM in the uterus: one is congenital and the other is acquired through previous uterine trauma (eg. curettage or previous pelvic operations), infection or trophoblastic disease. Congenital AVM is extremely rare, whereas acquired AVM is increasing in incidence. This rare condition occurs most frequently in women of reproductive age. Such women present most commonly with PV bleeding but some present with life-threatening bleeding. Management of AVM is mostly conservative but may necessitate embolisation.
Case report
A 30-year-old female (P3+1) presented at the emergency department at 6+ weeks gestation with mild pain and PV bleeding; following a scan, she was discharged home. She subsequently presented at the early pregnancy assessment unit (EPAU) for a further scan to confirm dates and the viability of her pregnancy. She was diagnosed with a missed miscarriage at 7+3 weeks and a plan was made for medical management. She received mifepristone and full doses of misoprostol, neither of which had any effect for two days. She was then booked for an evacuation of retained products of conception (ERPC). Her haemoglobin (Hb) levels were 12g/dl. During the ERPC, she bled > 2 litres within 25 minutes and required four units of blood transfusion.
The patient was managed via ERPC under ultrasound (US) guidance and then via a Foley catheter in her uterine cavity, filled with 30ml. The bleeding stopped and the catheter was removed after 24 hours. There was minimal bleeding and the patient was discharged home on day two with Hb 9.6g/dl and on oral iron.
 (click to enlarge)
(click to enlarge)

 (click to enlarge)
(click to enlarge)