NUTRITION
Tackling malnutrition among older patients
Early identification and treatment of nutrition problems can lead to better quality of life and improved outcomes in care of the elderly
April 14, 2016
-
Malnutrition is an important consideration in care of the elderly. It has a high prevalence in care homes and hospitals, but is also a risk for many elderly living at home. It impacts on quality of life, increases morbidity and incurs substantial financial costs associated with increased disease burden, nutrition support and increased length of hospital stay. This article reviews the causes and consequences of malnutrition in the elderly, how to identify those at risk, and intervention strategies to reduce prevalence.
In the UK it is estimated that 12% of over 65s living in the community are at high or medium risk of malnutrition. The prevalence is reckoned at 20% among those in residential accommodation and up to 40% in those admitted to hospital.1
In a study of meals-on-wheels recipients in Ireland, over one-third of recipients (38.5%) were malnourished or at risk of malnutrition and over half (52.3%) were overweight or obese.2
Causes
The risk of malnutrition increases with age and number of comorbidities.3 The multiple causes of malnutrition in the elderly include:
• Physiological decrease in appetite and food intake that accompanies normal ageing
• Reduced taste and smell
• GI side effects of prescribed medications
• Acute and chronic disease
• Poor dentition
• Age-related achlorhydria
• Social factors such as poverty and isolation
• Psychological factors such as depression and cognitive decline
• Physical factors such as poor vision and reduced mobility.
In an Irish study of community-dwelling 60 to 92-year-olds, the strongest predictors of abnormal nutritional status were poor mobility and lack of social support. Other significant predictors of nutritional risk were age and deprivation.4
Data from the ELDERMET study in Ireland indicate that the diet of community-dwelling elderly individuals is sub-optimal, particularly among elderly males. A high rate of overweight/obesity was observed and consumption of energy-dense, low-nutrient foods was excessive among this population group. Older subjects (≥ 75 yrs) consumed significantly more desserts/sweets than younger elderly (64 to 74 years old). Intakes of dietary fat and saturated fat were high while dairy food consumption was inadequate in both males and females. Elderly females typically had a more nutrient-dense diet than males. A considerable proportion of subjects, particularly males, had inadequate intakes of calcium, magnesium, vitamin D, folate, zinc and vitamin C.5
Consequences of malnutrition
Malnutrition leads to a depletion of body stores of nutrients and loss of muscle mass (secondary sarcopenia). This in turn has many consequences including:
• Increased infections, delayed wound healing, increased surgical complications
• Increased hospital length of stay
• Increased hospital mortality
• Delayed rehabilitation and convalescence
• Reduced functional capacity and quality of life
• Increased GP visits and increased re-admissions to hospital – high social cost
• Higher healthcare costs.
Up to 70% of elderly patients are discharged from hospital weighing less than when they were admitted. This results in a ‘malnutrition carousel’ of more GP visits and subsequent increased risk of re-admission.6
Malnutrition and dementia
There is a strong association of malnutrition with dementia. Often the first sign of cognitive decline to become apparent to an older person’s relatives is self-neglect with resulting inadequate diet and weight loss. A recent study in Cork revealed that patients admitted to acute hospitals with dementia, were older and frailer, with higher comorbidity, malnutrition and lower functional status.7
Conversely, there is increasing evidence that malnutrition may be a contributory cause of dementia. Low intake of folic acid, vitamin B12 and long chain n-3 fatty acids of marine origin has been shown in observational studies to be associated with higher risk for Alzheimer’s disease.
A review of long-term intervention studies has shown that adherence to a Mediterranean diet reduces the risk of developing dementia.6 Recently a number of studies have found a link between dementia and vitamin D deficiency.8
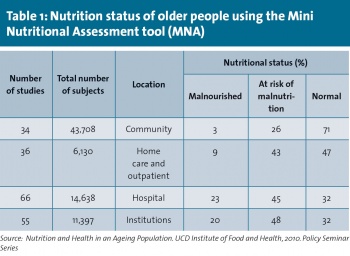
Identifying older adults at risk
A range of simple and validated screening tools can be used to identify malnutrition in older adults, eg. MST, MNA-SF and MUST (see example in Table 1).3 The Royal College of Physicians UK has identified nutritional screening as an integral part of clinical practice.1 Older adults should be screened for nutritional issues at diagnosis, on admission to hospitals or care homes and during follow-up at outpatient or GP clinics, at regular intervals.
A key barrier is that many GPs and nursing homes may either have no weighing scales or may not routinely weigh patients on admission or thereafter. This results in a failure to notice or act on any weight loss in older patients.
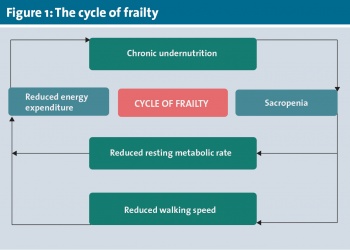
Malnutrition and sarcopenia
The ‘cycle of frailty’ (see Figure 1) has been described,6 and related to this is the new concept of a malnutrition-sarcopenia syndrome, in which malnutrition aggravates and accelerates the intrinsic sarcopenic process.
 (click to enlarge)
(click to enlarge)

 (click to enlarge)
(click to enlarge)